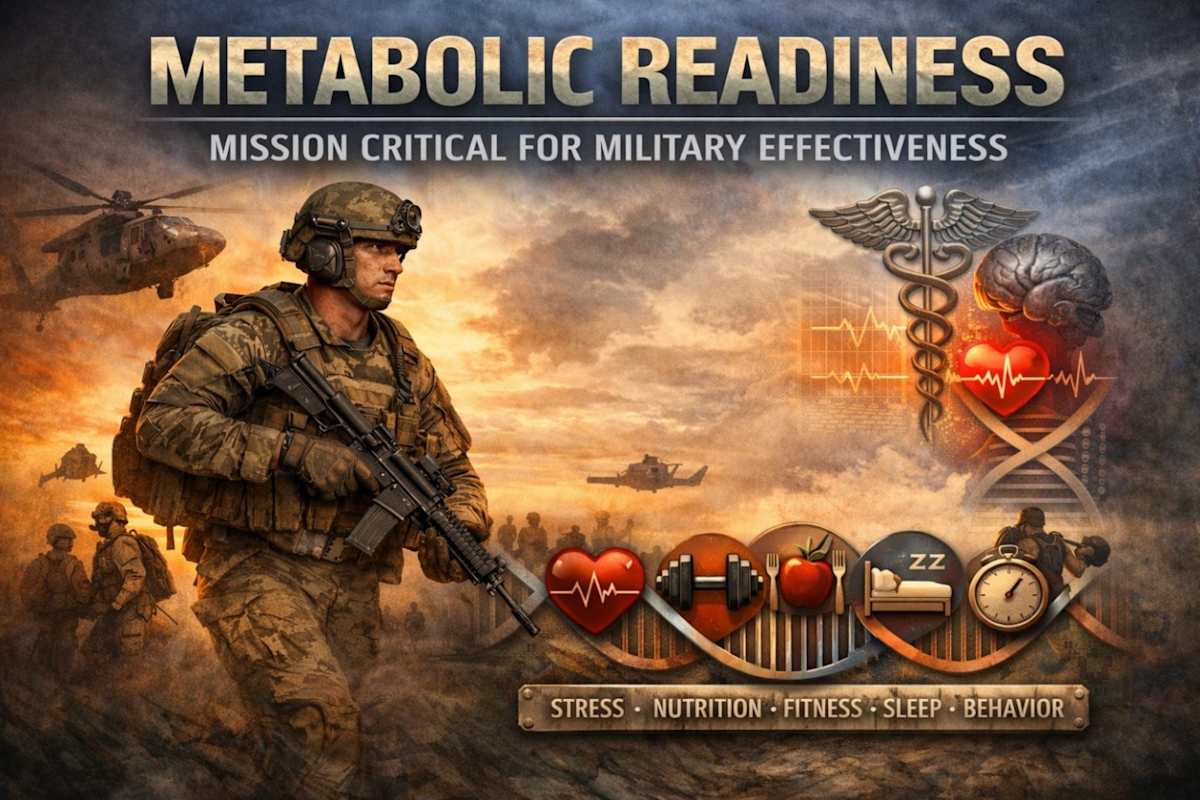
Metabolic dysfunction increasingly threatens accession eligibility, deployability, and long-term force health protection. Obesity prevalence among U.S. adults exceeds 42%, and cardiometabolic disease is rising among military-age Americans. Chronic stress, sleep deprivation, nutritional quality, and muscle mass preservation are interdependent determinants of metabolic resilience. Current approaches emphasize weight standards and aerobic conditioning but insufficiently address integrated endocrine, behavioral, and recovery domains. This commentary proposes a doctrinal shift: metabolic stewardship must be codified as an operational readiness imperative. By integrating stress mitigation, resistance training, sleep discipline, behavioral conditioning, and nutritional reform into force health protection programs, military medicine can preserve deployability and reduce downstream morbidity. The time has come to treat metabolic discipline not as aesthetics, but as operational preservation.
INTRODUCTION
The United States military depends upon a physically and cognitively resilient force. Yet the nation from which the force is drawn is experiencing unprecedented metabolic disease burden. According to the National Center for Health Statistics, adult obesity prevalence reached 42.4% in 2017–2018.¹ Severe obesity continues to rise.
These statistics are not abstract. They directly influence accession eligibility. Department of Defense accession data consistently demonstrate increasing disqualification rates related to excess body weight and associated comorbidities. Elevated body mass index correlates with increased musculoskeletal injury during initial entry training and predicts attrition.
Beyond accession, excess adiposity contributes to metabolic syndrome, hypertension, dyslipidemia, obstructive sleep apnea, insulin resistance, and cardiovascular disease. These conditions degrade endurance, recovery, and cognitive clarity—core pillars of operational performance.
This commentary argues that metabolic stewardship must be formally reframed as operational doctrine within military medicine.
THE ACCESSION CHALLENGE
The pool of eligible recruits is shrinking. National obesity trends directly narrow the eligible population. Elevated BMI and metabolic comorbidities reduce accession eligibility and increase waiver complexity. Service members entering training with excess body fat are at increased risk for stress fractures, overuse injuries, and attrition. Musculoskeletal injury remains a leading cause of lost training days and limited duty across services.
Early metabolic conditioning programs—pre-accession strength training, structured nutritional guidance, and sleep hygiene education—could expand eligibility and reduce attrition rates.
METABOLIC PHYSIOLOGY IS OPERATIONAL PHYSIOLOGY
The body is an integrated endocrine system. Operational performance depends on its stability.
Stress Physiology
Epel et al. demonstrated that chronic stress is associated with central adiposity independent of caloric intake.³ Elevated cortisol promotes visceral fat accumulation and insulin resistance. Operational tempo, leadership burden, financial strain, and family separation activate sympathetic pathways. Without structured recovery, chronic activation becomes endocrine dysfunction. Stress mitigation training must be viewed as metabolic protection.
Sleep Deprivation
Spiegel et al. demonstrated that sleep restriction decreases leptin and increases ghrelin, promoting hunger.¹⁰ Patel and Hu confirmed that short sleep duration predicts weight gain.¹¹ Sleep restriction also impairs insulin sensitivity, executive function, and emotional regulation. Chronic sleep deprivation degrades both metabolic and cognitive readiness. Sleep discipline must be codified as readiness doctrine.
Resistance Training and Muscle Preservation
Lee et al. demonstrated that physical inactivity accounts for approximately 9% of premature mortality.⁶ Ruiz et al. demonstrated that muscular strength independently predicts mortality.⁷ Muscle tissue is metabolically active. It enhances insulin sensitivity, improves resting metabolic rate, and protects joint integrity. Sarcopenic obesity increases injury risk and metabolic vulnerability. Resistance training is preventive medicine.
Nutritional Quality
Ultra-processed foods are associated with increased cardiovascular disease risk.⁸ High fructose intake increases visceral adiposity and lipid abnormalities.⁹ Operational feeding systems must prioritize protein adequacy, fiber intake, and glycemic stability.
Behavioral Conditioning
Wing and Phelan demonstrated that long-term weight maintenance depends on behavioral consistency.⁴ Butryn et al. confirmed that behavioral therapy improves durability.⁵ Military culture already reinforces identity-based discipline. Extending that framework to metabolic stewardship aligns naturally with doctrine.
DHA AND FORCE HEALTH PROTECTION CONTEXT
Defense Health Agency initiatives increasingly emphasize performance optimization and preventive care. However, metabolic disease remains a significant contributor to limited duty profiles and long-term Veterans Affairs burden. Metabolic syndrome increases lifetime healthcare utilization. Early intervention during active service reduces downstream costs and preserves deployability. A doctrinal shift would align preventive medicine, performance optimization, and operational leadership under a unified metabolic readiness framework.
PROPOSED DOCTRINAL SHIFT
- Institutionalize resistance training education across accession pipelines.
- Integrate structured stress mitigation modules within leadership development courses.
- Codify sleep discipline standards within readiness policy.
- Reform dining facility procurement toward reduced ultra-processed food reliance.
- Embed behavioral therapy tools within primary care preventive visits.
Metabolic stewardship must be treated as mission-critical.
STRATEGIC CONCLUSION
The military has historically led public health advances. From infectious disease control to trauma resuscitation doctrine, operational necessity has driven innovation. Metabolic dysfunction is now a readiness threat. Evidence demonstrates that stress physiology, sleep regulation, muscle mass preservation, nutritional quality, and behavioral identity are interdependent determinants of metabolic health. The question is not whether obesity affects readiness. It is whether doctrine will evolve to confront it. Metabolic discipline is not cosmetic. It is operational preservation.
CONFLICT OF INTEREST
The author declares no conflicts of interest.
FUNDING
None.
DISCLAIMER
The views expressed are those of the author and do not necessarily reflect official policy or position of the Department of War or the U.S. Government.
REFERENCES
- Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief. 2020;360:1-8.
- Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors. Arch Intern Med. 2011;171(15):1349-1356. doi:10.1001/archinternmed.2011.208
- Epel ES, McEwen B, Seeman T, et al. Stress-induced cortisol secretion and central adiposity. Proc Natl Acad Sci U S A. 2000;97(15):8629-8634. doi:10.1073/pnas.97.15.8629
- Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1 suppl):222S-225S. doi:10.1093/ajcn/82.1.222S
- Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am. 2011;34(4):841-859. doi:10.1016/j.psc.2011.08.006
- Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on mortality. Lancet. 2012;380(9838):219-229. doi:10.1016/S0140-6736(12)61031-9
- Ruiz JR, Sui X, Lobelo F, et al. Muscular strength and mortality. BMJ. 2008;337:a439. doi:10.1136/bmj.a439
- Srour B, Fezeu LK, Kesse-Guyot E, et al. Ultra-processed food intake and cardiovascular disease risk. BMJ. 2019;365:l1451. doi:10.1136/bmj.l1451
- Stanhope KL, Schwarz JM, Keim NL, et al. Fructose-sweetened beverages and visceral adiposity. J Clin Invest. 2009;119(5):1322-1334. doi:10.1172/JCI37385
- Spiegel K, Tasali E, Penev P, Van Cauter E. Sleep curtailment and hunger hormones. Ann Intern Med. 2004;141(11):846-850. doi:10.7326/0003-4819-141-11-200412070-00008
- Patel SR, Hu FB. Short sleep duration and weight gain. Sleep. 2008;31(5):619-626. doi:10.1093/sleep/31.5.619